Diagnostics & Treatment
Echocardiography, Stress-Echocardiography, Transesophageal Echo
Heart ultrasound (echocardiography or echo) is used to examine the mechanical properties of the heart: one can see how the heart pumps, how the heart valves close, how the segments of the heart walls move and whether the heart walls are thickened. Echo cannot provide exact information about the coronary vessels, i.e. whether there is a stenosis in a coronary vessel - this is usually checked using other methods. Echocardiography is therefore primarily used to determine the heart's pumping power or as we say ejection fraction (normal range of EF is >50-55%), i.e. whether the heart is able to pump out enough blood with each beat. Other important information is the function of the heart valves - are they calcified and narrowed, or are they not closing well – this is called valve insufficiency or regurgitation as part of the blood that passes the valve flows back and may damage the heart in the long run. However, mild valve regurgitation is a common finding and can be present in otherwise healthy people. In patients who have already had a heart attack or have a known coronary artery disease, certain findings can also be made on the basis of the motion of the heart wall, i.e. whether the heart walls move/shorten homogeneously and well, or whether a wall or a wall segment is unnormal.
Important: Echocardiography cannot rule out all possible heart problems. You can have a heart disease and an unremarkable echocardiography finding at the same time. One can also have a structurally and functionally healthy heart but suffer from cardiac arrhythmias, for example. Echo is therefore an important part of cardiac diagnostics, but cannot answer all questions and rule out all cardiac issues.
Stress-Echo
If we want to know how the heart or the heart walls behave when working under maximum stress - we may offer a so-called stress test: during a normal echocardiography, an i.v. drug is administered increasing the heart's pumping capacity and pulse. In this way, it is possible to simulate maximum cardiac output as under maximum physical stress. If there are relevant constrictions/stenosis of the coronary arteries, wall motion disturbances occur under 'stress' that are not present at rest. It is then reasonable to suspect that a circulatory disorder of coronary vessels may be present since it is the oxygen demand-supply-disbalance that leads to heart wall disfunction under stress. In the reverse shot, if the echo remains inconspicuous, no relevant constrictions of the coronary vessels are then suspected, since the heart walls motion is normal despite maximum stress.
Transesophageal Echocardiography
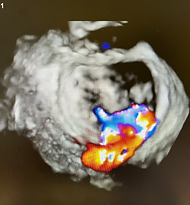
TEE or TOE is echocardiography carried out via the esophagus. At the tip of the probe is an ultrasound head that is able to send signals through the wall of the esophagus and, being anatomically close to the heart, can produce a much better image quality and different angulations the "normal" echo (TTE) cannot or may not perform well enough. The examination can be carried out with or without anesthesia and the probe is quite similar to the one in gastroscopy. This method is often used in patients with atrial fibrillation to exclude thrombus in heart chambers. TEE can also provide important information on heart valves prior to valve repair procedure or to quantify the valve dysfunction, when the TTE is not sufficient.



Cardiac - CT (Angiography of heart vessels with computed tomography)
Everyone knows computed tomography - X-rays in the tube that are directed at a specific organ and provide high-quality and high-resolution "slice" images. With CT, we can also visualize the coronary vessels of the heart in high resolution. This allows both to detect calcification of the vessels and to assess the narrowing/stenosis of the vessels. The examination is used when the probability of the presence of coronary artery disease is rather low and we would like to exclude it with certainty. The method is less suitable for patients with already known coronary heart disease. It is important to have a low pulse (preferably under 70 beats per minute) when performing the CT scan – in order to get a good image quality.



Cardiac - MRI
The only similarity between MRI and CT is that both examinations are performed in a tube. However, the MRI works with magnets and electromagnetic signals; in contrast to the CT, there are no X-rays and the examination therefore has no relevant risks. However, for a cardiac MRI you have to lie in the tube for about 40-60 minutes and if possible, not move. In addition, the breathing commands are somewhat strenuous; you have to hold your breath for 10-15-30 seconds at a time. On the other hand, the heart MRI offers a high resolution and excellent image quality. We can observe the heart from all levels and measure its functions. In addition, with the help of a contrast medium (usually gadolinium, which is a completely different contrast medium from what is normally used in coronary angiography or CT, i.e. not a medium containing iodine), diseases of the heart muscle can be recognised and differentiated. The MRI is also considered the gold standard for determining ejection fraction of the left ventricle. Similar to the stress echo, an artificial "heart stress" can be induced with the help of a drug and we can see how the heart walls or the blood flow to the heart muscle behave. In principle, almost all questions concerning heart diseases can be answered by means of cardiac MRI, but cardiac MRI also has limitations: Heavily overweight patients, patients with claustrophobia, patients enable to lie still or hold their breath. Certain arrhythmias can also affect the image quality. And MRI does not play a relevant role in the diagnosis of cardiac arrhythmias.



Coronary Angiography (incl. Stenting, Rotablation, IVUS, CTO-Interventions, protected-PCI with Impella, rFR/FFR-Measurements)
This is the so-called invasive imaging, where the coronary vessels are directly displayed. A thin catheter is advanced via arm or leg arteries to the heart level, where it is placed in the coronary vessels and displayed under X-ray fluoroscopy with contrast medium. Here it is possible to see exactly which vessels are narrowed and also to classify/quantify the stenosis. It is known that treatment with a stent can only be carried out without further measurements if the narrowing is more than 90% of the lumen. If the stenosis is measured as less than 90% it is possible (and actually obligatory) to determine the blood flow in the vessel and thus see whether the flow before the stenosis and after the stenosis are approximately the same (and thus the narrowing of the vessel does not contribute to a reduction in flow) or whether there is a relevant difference - then even a stenosis of less than 90% can be classified as relevant and, if necessary, treated with a stent. So, not every narrowing should be treated with a stent. The treatment with stent will usually be done in the same session, using special catheters, wires and balloons. The stent is made of different metals and stays in the vessel forever, but over time it is covered by the vessel wall with a thin layer, so that after a certain time it is in the vessel wall.
Coronary angiography is used to examine patients who have either definitely suffered a heart attack or have symptoms that clearly indicate the presence of coronary heart disease or if a further examination such as stress echo, stress MRI or coronary CT has already detected it. Sometimes, however, the examination is also carried out in order to enable further operations on the heart or to exclude coronary artery disease as a risk feature, sometimes also in order to be allowed to give certain medications that are contraindicated (not allowed) in patients with coronary artery disease.
Possible complications: As manipulations in the aorta and in the very thin coronary vessels are carried out, complications may occur as in any other field of medicine. One can thus injure the vessels, cause a heart attack or a stroke. These are the most dangerous complications and are extremely rare (<1%). Occasionally, there may be bleeding complications from the puncture site (access route to the heart), which can usually be managed well.



Electrophysiological Study:
EP is used for many cardiac arrhythmias (heart rhythm disorders). It is an invasive diagnostic as well as therapeutic method for the treatment of numerous rhythm disorders where drug therapy is either not sufficient or not desired.
In certain respects, EP study is similar to a cardiac catheterisation: a catheter is inserted into the heart via vessels and under fluoroscopy. The access route in EP study is the venous system and not the arterial system. Through the veins we get to the right heart, where a lot of information about the electrical properties of the heart can be obtained with the help of various electrodes. If a rhythm disorder is running, one can see what kind of rhythm problem it is and where it comes from, whether it is on the right or left side of the heart. After finding the spot, we may ablate the lesion with a radiofrequency or a cryoballon (with a heat or cold). There are also some standard spots that are usually being ablated in atrial fibrillation or atrial flutter. As any kind of invasive intervention on heart, this method also has its limitations (not every rhythm disorder can be treated and not every treatment is successful) as well as risks that are similar to those of coronary angiography.



Pacemaker, Defibrillator, resynchronisation Therapy
These are electronic devices that can stimulate the heart (pacemakers), eliminate a malignant cardiac arrhythmia in the case of sudden cardiac death with an "electric shock" (defibrillator) or synchronise a heart that is not pumping synchronously (CRT). The indication for the respective device is checked and set on the basis of guidelines, the criteria are clearly defined and cannot be adjusted arbitrarily or as desired. Usually, electrodes are advanced through arm/breast veins under X-ray control into the heart, where they are twisted into the heart muscle and then connected outside the body to the respective device, leading to an electrical connection between the device and the heart. The device is then placed in a subcutaneously prepared "pocket" in the chest area, after which the pocket is sewn. There are now also devices that work without electrodes and lie directly in the heart (very small pacemakers) or devices where the electrode lies in the chest under the skin (subcutaneous defibrillator). However, these devices do not fit every patient/every issue and should be chosen carefully. In general, we differentiate between pacemaker-therapy for someone whose pulse is very low or pauses appear occasionally, ICD- or Defibrillator-therapy for malignant arrhythmias to prevent sudden cardiac death (preventive therapy) as well as pacing the heart in a manner that it contracts synchronously (in patients with so called left-bundle-branch-block and low ejection fraction).

TEER (Repair of cardiac valves without a surgery)
This method is for repair of only certain valve regurgitations, where the valve leaflets are "stapled" together at certain points. The procedure is done through a groin access, where a special device is brought through the veins into the heart, then under fluoroscopy and transesophageal echo, the exact location of the regurgitation is documented and an attempt is made to catch the corresponding parts of the leaflets with a "clamp" and fix them to each other. The procedure is very complex and not suitable for all types of valve insufficiencies. Selection is the key to success and should be done carefully. The procedure is considered when surgery is not an option due to risks. Despite the minimally invasive nature of the procedure, it is done under anesthesia to achieve a better result. Patients are usually ready for discharge the next day or the day after. Whether the valve regurgitation disappears completely or a mild regurgitation remains depends on many factors and cannot be guaranteed in advance.



Holter ECG and 24h Bloodpressure Measurements
Those are diagnostic methods that are widely available in all parts of the world and usually of the same quality. In patients with rhythm disorders we usually need more information than just an ECG strip so that a 24h ECG may provide such an information, especially if we are "lucky" to capture the rhythm disorder within those 24h, where the patient wears the holter ECG.
The Bloodpressure measurement within 24h provides a more precise picture of how good or bad the current hypertension treatment works. If the average BP is too high, that this finding can lead to a change in therapy. Usually this diagnostic method is provided from family doctor.

